REFLUX DISEASE
Reflux occurs when the valve between the oesophagus and the stomach doesn’t function properly, allowing stomach fluid containing variable acid to escape into the oesophagus. This may cause discomfort, heartburn and a sense of fluid rising behind the breastbone (regurgitation).Most reflux patients are well treated by medication. Many patients choose not to continue with long term drug treatment in light of the possible link between long term use, osteoporosis, gastric cancer and increased bone fracture rates, amongst others.
A proportion (20-30%) of patients develop breakthrough symptoms despite maximal medical therapy and are considered to have failed medical management.
Symptoms include:
- Heartburn
- Stomach fluid regurgitation (without necessarily vomiting) often into the throat
- Cough
- Sore throat
- Chest pain
- Pulmonary inhalation
- Nocturnal sleep disturbance, sitting up to sleep
- Occasional choking food jamming with swallowing
- Voice trouble
Any change in heartburn or food sticking on swallowing, or pain on swallowing should be investigated quickly. These patients are 'fast tracked' to endoscopy to exclude development of cancer.
Reflux Medicine Failure
Often as the medication ‘wears out’ patients need to increase their doses, which often incompletely help.
Reflux of vomit can occur at night and sleep may be disturbed.
A chest ache can often occur, raising heart concerns. Typically, the chest ache will occur at the same time as heartburn occurred previously.
Heartburn and regurgitation may persist. There may also be difficulty or pain on swallowing and food may stick. It is important to quickly check these two problems as alternatively the cause may be cancer.
Reflux Related Cough and the Throat
Airway problems can occur with reflux disease.
Symptoms include:
- Cough
- Weak voice
- Throat soreness / dry throat / 'lumpy' throat
- Throat clearing / mucous throat
- Occasional inhalation of stomach contents (aspiration) particularly at night or when lying down
- Chest infections
This condition usually responds poorly to medication, even in high doses. It is frequently caused by substance other than acid (such as bile, gas or peptic juices). More frequently double dose medication and occasionally surgery may be of benefit. If medication has not helped after 6-8 weeks it should be discontinued.
Surgery is strongly indicated if there is a history of aspiration and choking as it may cause pneumonia and lung disease.
Alarm symptoms such as food sticking, weight loss, anaemia or pain when swallowing require urgent investigation.
For information on cough, visit the International Society for the Study of Cough (ISSC) page: http://www.issc.info/cough.html
Reflux and Singers
Singers have a special problem due to the pressure placed on the diaphragm during singing. Reflux can occur just by straining. It can cause the voice to be damaged.
Reflux and the Lung
Increasing shortness of breath and chest infections are being seen with small amounts of reflux contaminating the lung. This can be very hard to diagnose and requires extensive testing. Use of Proton Pump Inhibitor (PPI) medication for reflux is associated with more chest infections as reduced acid reflux fluid contains more bacteria.
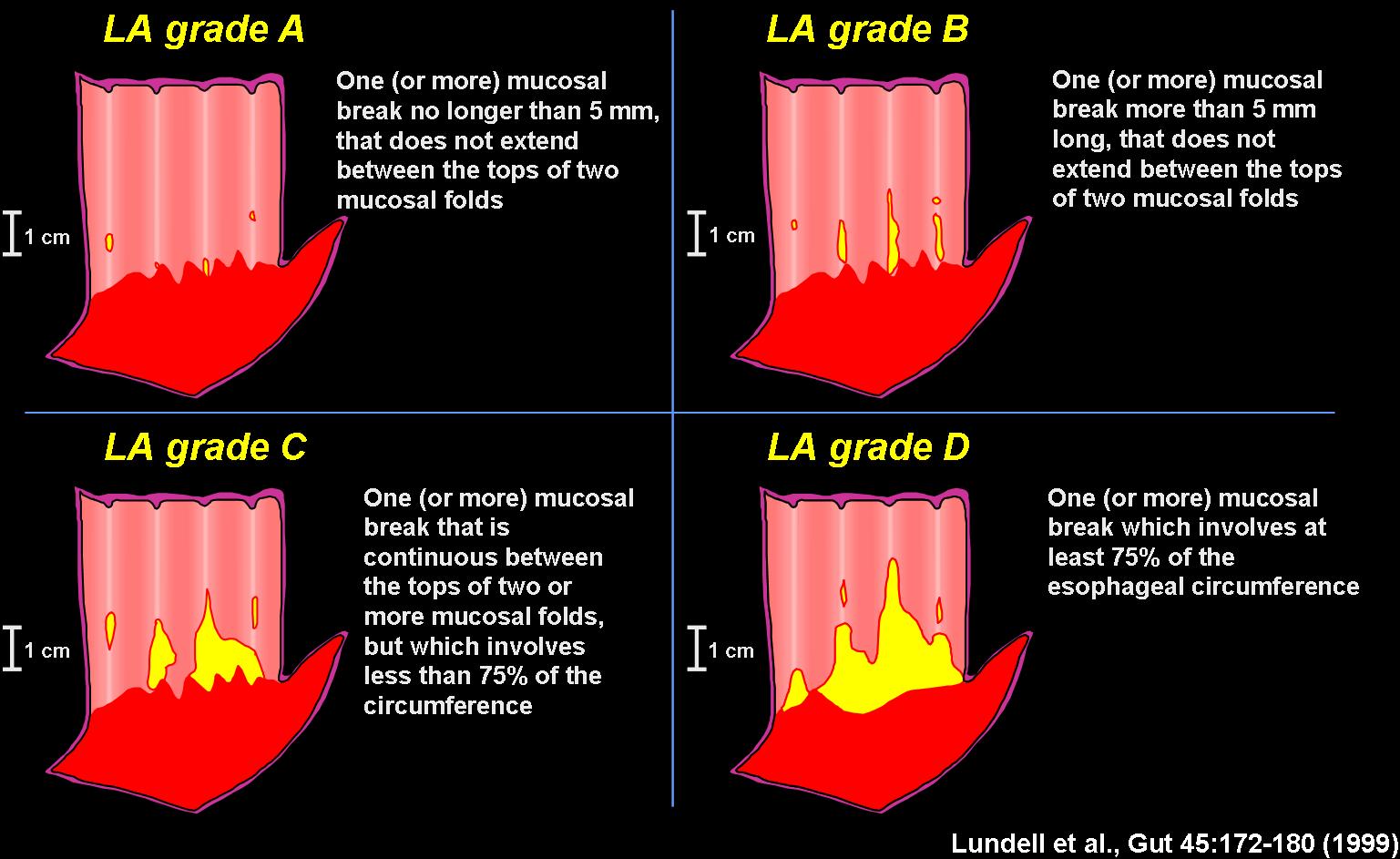
The Los Angeles Classification of Gastroesophageal Reflux Disease
SWALLOWING DIFFICULTIES
Food may not pass through the oesophagus properly, becoming blocked. This may be caused by several conditions. Achalasia and oesophageal spasm disorders occur. Ineffective oesophageal peristalsis (IEM) is common. Diagnosis occurs in our laboratory and various treatments can be offered (myotomy, dilatation, medication). Other causes of food jamming may be cancer, scarring, or inflammatory causes.Swallowing difficulties may have a number of different underlying causes including:
Achalasia
The oesophagus loses contractility and the lower valve does not open properly. It commonly causes chest pain and regurgitation of old food (not vomit) often containing slime, and there can be a sensation of food jamming. Cough is frequent. Surgery is available to relieve these symptoms.
Oesophageal Spasm
This condition often causes unusual chest pain, food jamming, or regurgitation. It is rare and can be confused with achalasia. We can perform tests in our laboratory to differentiate it. Various treatments may be of assistance.
Other motility problems
A number of other problems can also affect the “motility” of your oesophagus, that is, your oesophagus’s ability to carry food to the stomach:
- Ineffective oesophageal motility
- Subtypes of achalasia
- Presbyoesophagus
- Segmental spasm
- Immotility of the oesophagus (absent peristalsis)
- Scleroderma
Oesophageal Diverticulum
An oesophageal diverticulum is a small pouch that can develop in the oesophagus. It is a condition which occurs in several sites in the oesophagus and can cause significant symptoms. We can usually see them using a barium meal x-ray, and can usually be relieved by performing surgery. We treat all kinds of oesophageal diverticula (Zenkers, cricopharyngeal pouch and epiphrenic diverticulum).
The diverticulum is caused by an uncoordinated “squeeze” in the oesophagus which usually requires surgery to release the pressure, and removing the diverticulum usually helps the symptoms. It is very rare.
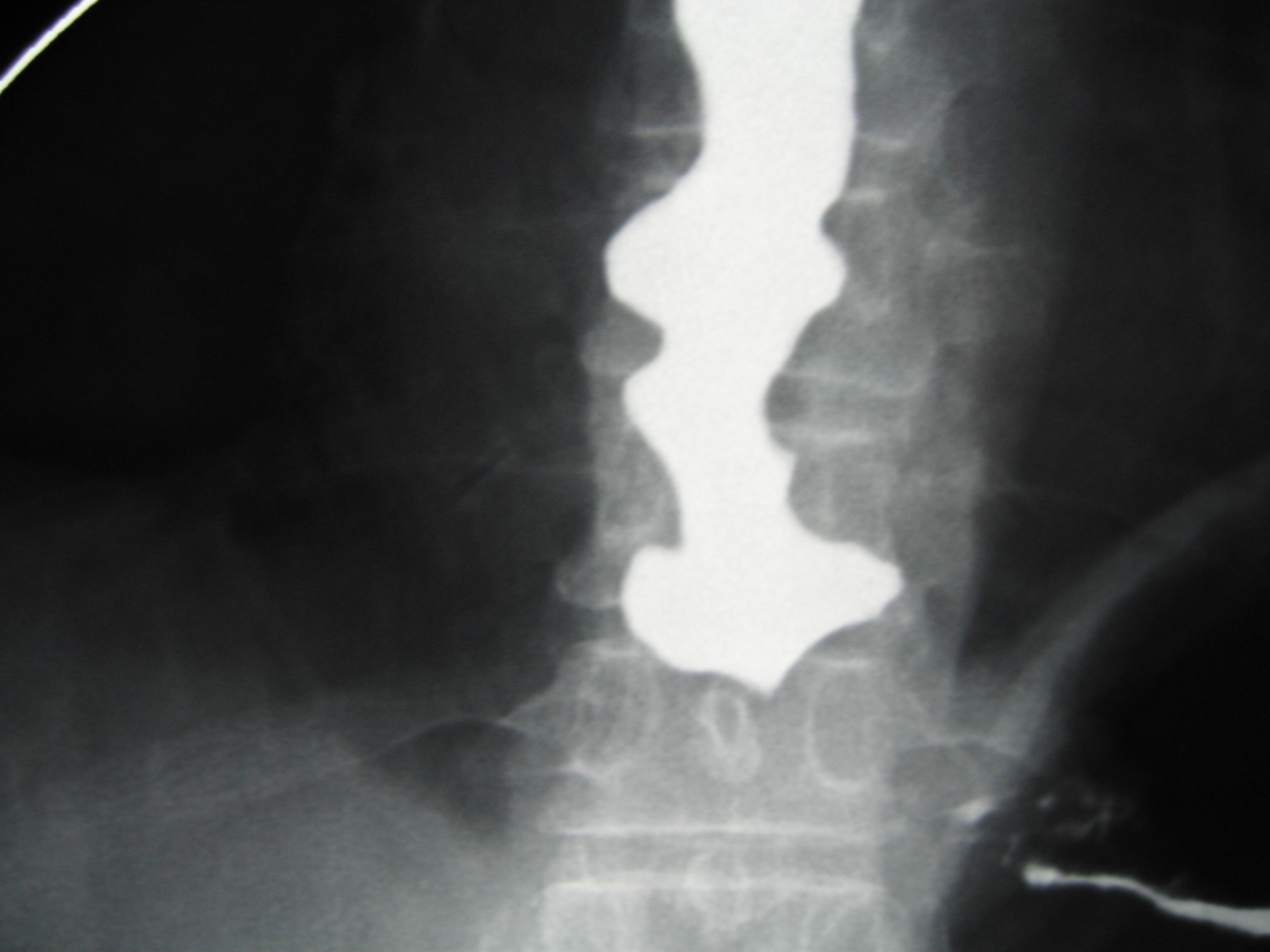
A Barium Swallow x-ray showing a “corkscrew oesophagus” caused by oesophageal spasm. Note the 'corkscrew' shape of the oesophagus in the centre of the image.
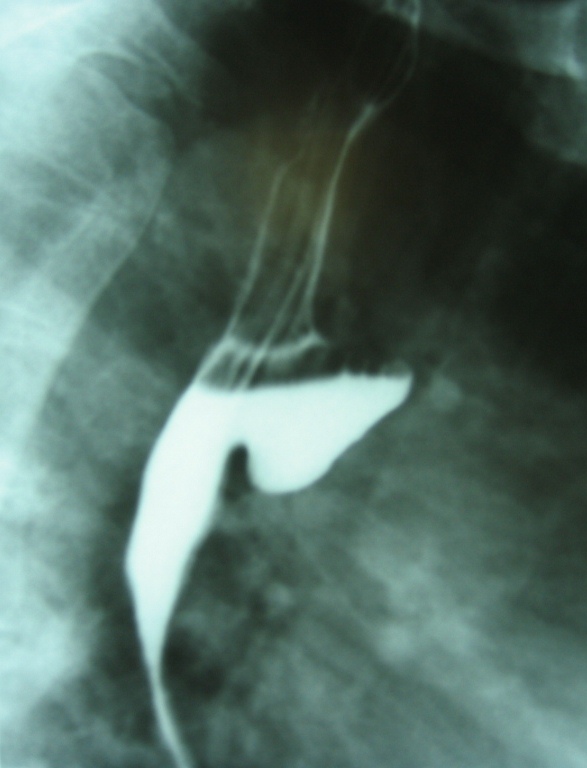

Barium Meal x-rays of an oesophageal diverticulum.
GALLSTONES
Gallstones occur in the gall bladder and are stone like concretions of cholesterol, bile pigment and sometimes calcium. They are one of the most common problems of the digestive system. For people who experience symptoms, removal of the gallbladder is usually the best form of treatment. Gallstones can cause complications such as pancreatitis or jaundice which is best avoided as they may be life threatening and lead to long times in hospital.Symptoms include severe pain in the low chest/upper abdomen which can be felt in the back and last longer than half an hour.
Gallstone induced pain is often confused for heart attack. Your local doctor will advise you as to whether gallstones are causing the pain and it is always wise to promptly have the heart checked. The best, and least expensive test to diagnose gall bladder stones and gallbladder disease is an ultrasound, as CT only shows 10%-20% of stones, and requires radiation.
GIANT HIATUS HERNIA
Giant hiatus hernia occurs when a large portion of the stomach rolls up into the chest. This causes different problems to reflux disease. It can strangulate which is very serious.Patients with very large hiatus hernia often do not have typical symptoms. The heartburn and regurgitation which was present in the past sometimes disappears as the hernia enlarges. It starts to get trapped.
Symptoms include:
- Difficulty swallowing
- Food jamming in the oesophagus
- Small appetite
- Chest pain after eating which mimics a heart attack (especially after a heavy meal)
- Unexplained anaemia
- Poor exercise tolerance
- Shortness of breath
- Palpitations
- Inability to eat and inanition
- Severe chest pain and shock due to strangulation
Medication in this case is only effective for reducing heartburn and does not fix the other symptoms and does not reduce the risks of strangulation. If your doctor has seen a hiatus hernia on your chest x-ray it is likely a dangerous one.
Dangers
- Severe bleeding from the stomach / ulceration
- Strangulation of the stomach hernia
- Possible fatality as a result of the above
Diagnosis
This condition can be partly recognised by its symptoms. The best form of diagnosis is by your local doctor performing a barium meal. Sometimes the situation is recognised on endoscopy, but it is frequently misinterpreted. Sometimes barium reports are not clear. Our group can review these by email.
Treatment
Treatment is by keyhole surgery and a 2 day hospital stay. Results have been excellent and the lethargy, shortness of breath and eating have been greatly improved. Risks of strangulation and life threatening complications are greatly reduced.
Visit our page on laparoscopic repair of giant hiatus hernia.
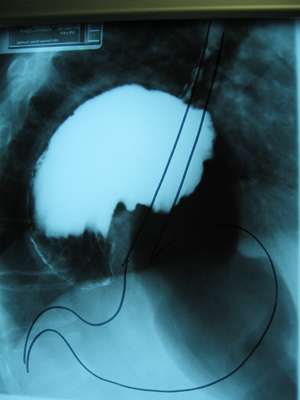
Barium meal of a twisted giant hiatus hernia with normal stomach position outlined in marker.
BARRETT’S OESOPHAGUS
This is a condition where the lining of the oesophagus changes and becomes potentially prone to an increased cancer rate.It is observed in patients with:
- Hiatus Hernia
- Heartburn
- Regurgitation
- Reflux
It is thought to be related to reflux of stomach content into the oesophagus. It is identified by endoscopy and often surveillance every three years is advised, by repeated endoscopy and biopsy.
Dysplasia refers to early changes in Barrett’s oesophagus that are precancerous. They can be found by endoscopy by taking many biopsies. There are different grades of dysplasia. High-grade dysplasia is particularly concerning for development of cancer.
Treatment:
Patients with any dysplasia in Barrett’s oesophagus can undergo endoscopy with ablation of the Barett's lining with the expectation that the risk of cancer will be reduced if not completely eliminated. The new technique of Halo® radiofrequency ablation is extremely promising and five-year results in very well respected articles are encouraging. Recovery time is minimal. We have been performing this procedure for many years.
Watch a video of Professor Falk performing a Barrett’s Ablation:
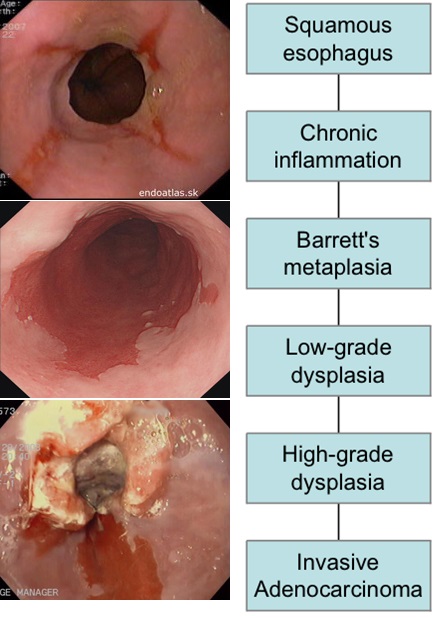
Evolution of Barrett’s and Cancer Picture and Diagram courtesy of Device Technologies.
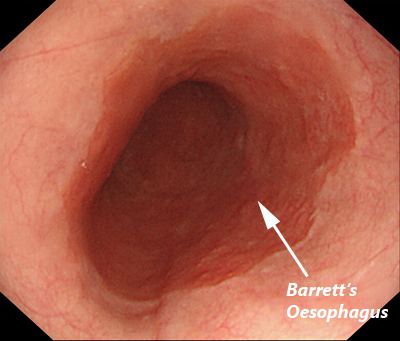
Oesophageal Mucosa Pre-HALO Treatment. Picture courtesy of Device Technologies
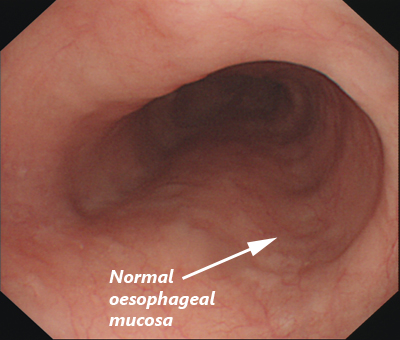
Oesophageal Mucosa Post-HALO Treatment – 2 years. Picture Courtesy of Device Technologies
OESOPHAGEAL CANCER
Oesophageal cancer can result from reflux disease. The continual escape of stomach acid into the oesophagus leads to inflammation, bleeding and ulceration of the skin-like lining of the oesophagus. This damage can cause changes in the cells (such as Barrett's oesophagus), which may lead to cancer. While smoking is a well known cause of oesophageal cancer, there are many other exacerbating factors including severe heartburn and obesity.Symptoms include:
- Sensation of food sticking in the food pipe
- Less reflux and heartburn (because of narrowing)
- Chest pain
- Loss of weight / anaemia
- Vomiting especially with blood
- Change in the pattern of reflux
Barrett’s Oesophagus can predispose the patient to cancer of the oesophagus. It is an increasingly common illness. Early diagnosis will lead to better prospects of cure. Oesophageal cancer can be cured if in the early stages.
Treatment
A combination of surgery with other techniques seems to offer the best prospect of cure. Treatment without surgery predominately relieves symptoms but does not result in lengthy survival. Some patients are not suitable for surgery. We have found removal of lymph nodes has markedly improved survival.
A high concentration of experience and high volume of cases performed by the surgeon is essential to increase the cancer cure rate and reduce the complication rate of what is a very large operation. As only diseases of the upper gastrointestinal tract are treated within this clinic a large number of patients are treated.
Management through a multi-disciplinary approach including radiotherapy, oncology, gastroenterology, dietetics and anaesthetics is vital. Cardiology and respiratory medicine are also often utilised.
Some patients are suitable for keyhole surgery. Professor Falk has developed techniques to minimise pain and to improve surgical cancer cure rates.
Treatment when surgery is not possible
The clinic treats many patients where surgery is for one reason or another is not advisable. Standard techniques are all available, however a number of alternatives can be targeted to individuals for different effect. Laser rebore is utilised in many cases. Laser has a great advantage of being symptomatically better treatment and has longer survival than stent placement. Internal radiotherapy can be done in other cases and can offer quite good control of disease (brachytherapy). Standard radiation and chemotherapy is often recommended. Oesophageal stents can be uncomfortable and we try to limit its use until absolutely necessary.
For more information on oesophageal cancer, visit this Cancer Research UK information page: http://www.cancerresearchuk.org/about-cancer/oesophageal-cancer
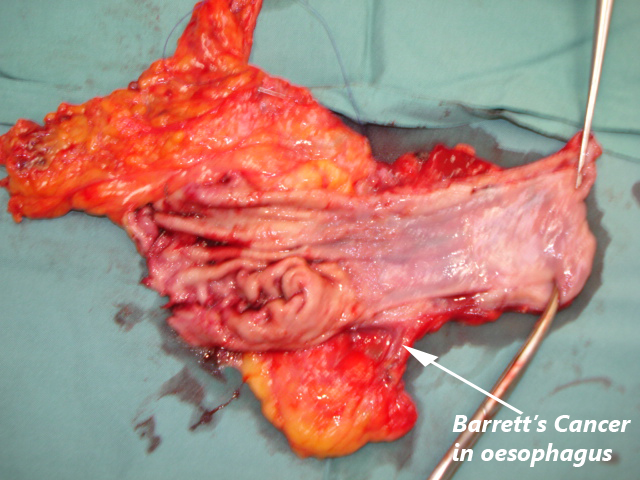
Oesophageal Cancer Removed
Barium Meal of Oesophageal Cancer
STOMACH (GASTRIC) CANCER
The combination of surgery with the removal of the cancer and draining lymph nodes offers improved survival. Outcomes are only acceptable when surgeons perform operations frequently, affecting both early complications and improving cancer survival results. Removal of lymph nodes in gastric cancer has shown that five-year survival is improved from 40%-45% to more than 65%. This is achieved by radical removal of the lymph nodes around the coeliac axis, hepatic artery, splenic artery and the pancreas (D2 resection).Particular training is required for management of the lymph nodes in gastric cancer. It requires a specialised oesophago-gastric surgeon.
Outcomes are only acceptable when surgeons perform operations frequently, affecting both early complications and improving cancer survival figures.
Some patients are suitable for key hole (laparoscopic) surgery for stomach cancer and this surgery can only be offered with good cure rates in a high volume setting.
For more information on stomach cancer, visit this Cancer Research UK information page: http://cancerhelp.cancerresearchuk.org/type/stomach-cancer
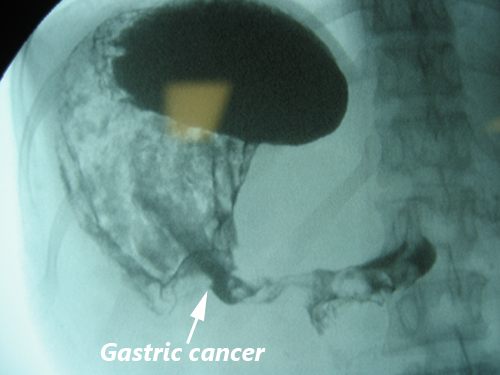
Barium meal of stomach cancer
GASTROINTESTINAL STROMAL TUMOUR (GIST)
Gastrointestinal Stromal Tumour (GIST) is a less frequent tumour that can occur in the stomach, oesophagus or bowel. It is sometimes found incidentally by endoscopy. It is not as malignant as stomach or oesophageal cancer however it can cause local problems and should be removed in most cases. In some specific situations, it can be observed over time rather than being removed immediately.Possible complications of not removing the GIST:
- Internal bleeding
- Can grow to a large size and spread
- Damage to increased amounts of stomach or bowel requiring more damaging surgery
Almost all of Professor Falk’s patients with this sort of tumour have only required keyhole surgery, have had an early recovery and required only two to three days in hospital. Most have returned to work within a few weeks.
Occasionally additional medical therapy is suggested but this is dependant upon laboratory examination when the tumour is removed. The rate of mitosis (growth) and serological markers (C-KIT, DOG1) are utilised in an algorithm to recommend what, if any, appropriate extra treatment is required.
Treatment
Almost all patients are treated by keyhole surgery with excellent results. Sometimes secondary disease can occur. Adjuvant chemotherapy (i.e. chemotherapy after surgery) is recommended for some patients.
We can minimise the resection by removing the least amount of stomach possible, in order to reduce the side effects without reducing the cure rate.
For more information on Gastrointestinal Stromal Tumour (GIST), visit this Cancer Research UK information page: http://www.cancerresearchuk.org/about-cancer/soft-tissue-sarcoma/types/gastrointestinal-stromal-tumour-gist
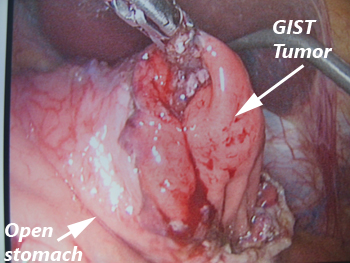
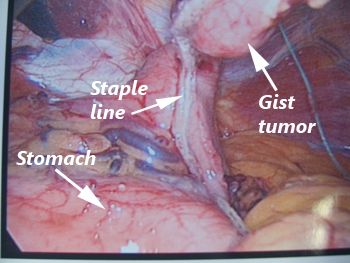
A GIST being removed laparoscopically (keyhole surgery).
For all appointments and enquiries contact us on:
FAX : +612 8580 5085