UPPER GI SURGERY
CHOLECYSTECTOMY (GALLBLADDER SURGERY)
Surgery for the removal of the gallbladder and/or gallstones is most frequently performed by laparoscopy. Patients are usually in hospital for one day or overnight.Stones that have escaped from the gallbladder and caused jaundice (yellow eyes, skin and dark urine) are often treated by removal at the time of keyhole surgery or by endoscopy.
We currently perform mini laparoscopic cholecystectomy in suitable patients using very fine instruments and incisions. Mini cholecystectomy results in less scarring and pain than traditional keyhole cholecystectomy. It can be performed as a day procedure.
Outcome
Most patients are completely cured of their pain. Complications are uncommon and are discussed prior to surgical recommendation. Diarrhoea and recurrent pain are extremely uncommon following surgery.
Balance of risks
The balance is in favour of removal of painful gallstones. It is more dangerous to allow the stones to become infected, cause pancreatitis or jaundice, or develop septicaemia. Very occasionally long standing gallstones may cause gall bladder cancer after many decades.
Gall Bladder Polyps
Most ‘gall bladder polyps’ are actually small, soft stones; however, a true fleshy polyp can cause cancer. Any suspicious polyp approaching 7mm should be removed for diagnosis to prevent cancer development. Polyps are often associated with gastrointestinal pain, and surgery fixes it in most situations.
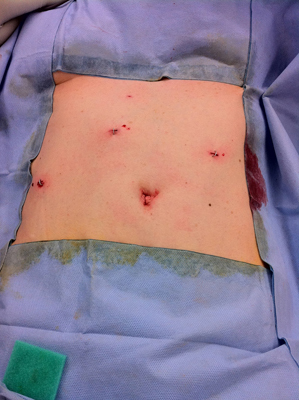
A Mini-cholecystectomy. Note the small 5mm incisions.
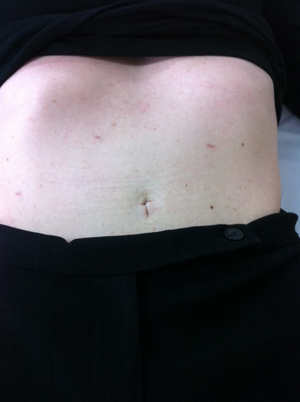
6 weeks later, showing the wounds have closed.
LAPAROSCOPIC REFLUX SURGERY (REFLUX SURGERY, ANTIREFLUX SURGERY)
For the past 20 years, surgery for the treatment of reflux has largely been performed by laparoscopic repair. Hospital stay is between one and two days and our complication rate is exceptionally low. There are now more than 3000 patients on our database who have had this surgery.Who is suitable for surgery?
1. Patients with continued symptoms despite medication
These include cough, sore throat, heartburn, chest pain, fluid regurgitation, pulmonary inhalation and nocturnal sleep disturbance.
2. Patients with very large Hiatus Hernia
These hernias can be life threatening and cause severe symptoms frequently, especially being short of breath.
3. Patients with abnormalities in Barrett’s Oesophagus
In combination with other management, surgery may be helpful in reducing cancer risk.
4. Patients concerned with side effects or long term problems of medication, or younger patients expecting a lifetime of medication.
These can include a decrease in bone density and osteoporosis.
Fundoplication
Fundoplication is the surgical technique utilised to reduce frequency and duration of reflux episodes, fixing heartburn and regurgitation of stomach content. It has evolved and improved over many years leading to a great reduction of side effects and good durable outcomes.
Recovery
Most patients are out of hospital in 1-2 days and require very little pain relief. It is often reasonable to drive at one week and work thereafter at a sedentary job.
Results
We perform fundoplication similar to the "Nissen" but designed to be to be robust enough to last and loose enough to minimise side effects. Much has been made of side effects, but we have found them to be infrequent after 6 weeks and not greatly troubling. They are, however, unpredictable. These consist of reduced belch, variable ability to vomit, sensation of food sticking in the valve, intermittent bloated sensation and increased flatus. In our most recent published report 95% were pleased to have chosen surgery even after 5 years duration.
For reflux surgery to be successful, it must be the key focus of the surgeon. High volume practice leads to effective surgery in the right patients (by testing), and limited digestive side effects. This group focuses on disease of the stomach and oesophagus almost exclusively, leading to better results.
Revision Surgery
Revision surgery has been performed on patients who have had operations (predominately elsewhere) requiring correction. This can be performed by keyhole surgery (laparoscopy), but is dependant on difficulty; standard open surgery may be necessary.
Watch Professor Falk perform a laparoscopic fundoplication:
LAPAROSCOPIC REPAIR OF GIANT HIATUS HERNIA (HIATUS HERNIA SURGERY)
Giant hiatus hernias symptoms are heartburn and regurgitation but also symptoms of poor exercise tolerance and shortness of breath. The most common symptom however is chest pain, which can feel like it is a heart problem. Inability to eat a full meal is also a common symptom. Giant hiatus hernias can twist and strangulate causing bleeding, chest pain, collapse, rupture or loss of blood supply. This can occur after many years of considerable discomfort as the hernia becomes larger over time. It is important to treat giant hiatus hernias early, as in some older patients they can be fatal. The hernia may twist the oesophagus (swallowing tube) and cause food to jam.Repair of this condition has been performed by this service for nearly 20 years. It usually results in patients only needing to be in hospital for 1-2 days. There is little pain and recurrences have virtually been eliminated. Early return to work and activity, within days, is expected. Few complications occur. Satisfaction is reported in our service as high, more than 95% of patients content.
In our experience of more than 700 giant hernias, repair is best performed by laparoscopic (keyhole) surgery. This is technically difficult and not all surgeons are comfortable performing this operation. Some surgeons use mesh to repair the hole in the diaphragm, but recent articles have confirmed that mesh repair is associated with particular risks.
The complication rate of laparoscopic repair in our clinic is about 4% and about 14% if open surgery is performed. We would usually recommend laparoscopic repair if possible but not everybody is suitable for keyhole approach.
There has been concern expressed in medical publications that these hernias can return, but several operations have demonstrated a satisfactory repair rate, similar to the clinic experience of 2% large recurrence and minor abnormalities in 8%.
Quality of life following surgery has been found to be greatly improved, often with comfort and exercise ability trebling.
Watch Professor Falk perform a giant hiatus hernia repair:
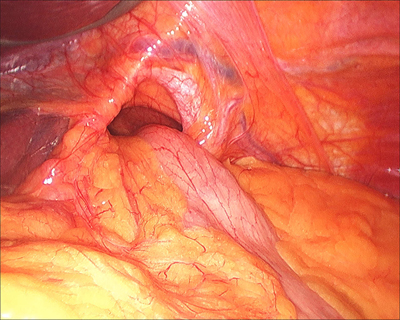
Laparoscopic Fundoplication for Large Hiatus Hernia showing a giant hiatus hernia with stomach passing through the hole in the diaphragm.
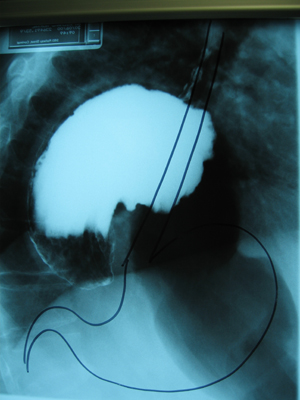
Barium Meal of a Giant Hiatus Hernia with normal stomach position showing.
OESOPHAGEAL CANCER RESECTION (OESOPHAGEAL CANCER SURGERY)
Otherwise known as an Oesophagectomy. This is a surgical procedure used to treat cancer of the oesophagus. Our series of patients show superior results using the technique of two-field lymph node removal. Some patients are suitable for abdominal or thoracic operation by keyhole (minimally Invasive oesophagectomy) with a view to early recovery.Statistics
Surgery Cure Rate (approximation)
Standard Surgery 25%
Combination of surgery and chemotherapy 35%
Combination of surgery, chemotherapy and lymphadenectomy (our approach) 45%
Investigative workup
Patients are investigated fully using best modalities to ensure appropriate recommendations. Endoscopic ultrasound, PET scanning, CT scanning, laparoscopy and sometimes bronchoscopy are utilised before surgery.
Procedure
The usual procedure removes draining lymph nodes and resects the tumour with a “margin” of clearance to achieve the best results. It is a large operation and is best managed in ICU for a few days following.
Enhanced anaesthesia / analgesia / pain management
Recent adoption of newest techniques to leave small tubes in the abdomen has been highly effective in delivery of pain medication. Similar approaches to the thoracic wound have had equally effective results. Results are most promising.
Chemotherapy / Radiotherapy
Most patients are offered “neoadjuvant” chemotherapy treatment to downstage tumour with a view to more curative surgery. Combination therapy is established as best practice but is not required all patients.
For more information on oesophageal cancer, visit this Cancer Research UK information page: http://www.cancerresearchuk.org/about-cancer/oesophageal-cancer
GASTRECTOMY (GASTRIC CANCER SURGERY, STOMACH CANCER SURGERY)
High VolumeOutcomes are only acceptable when surgeons perform operations frequently, affecting both early complications and improving cancer survival figures. Professor Falk has performed over 500 stomach cancer related operations.
Laparoscopy/Keyhole Surgery for stomach cancer
Some patients are suitable for keyhole (laparoscopic) surgery for the treatment of stomach cancer.
Lymphadenectomy
The combination of surgery with the removal of the cancer and draining lymph nodes offers improved survival. Removal of lymph nodes in gastric cancer series has shown that five-year survival is improved from 40%-45% to more than 65%. This is achieved by radical removal of the lymph nodes around the celiac axis, hepatic artery, splenic artery and the pancreas.
Enhanced Analgesia
Recent adoption of state of the art anaesthetic and pain techniques has enabled surgery with a cut to be performed with minimal discomfort to the patient. Small (1 mm) tubes are left in the abdomen to eliminate pain. It is highly effective, but varies between patients.
Neoadjuvant Chemotherapy
Many patients are suitable for combination therapy (chemotherapy and/or radiotherapy before surgery) which is 13-15% more likely to cure the cancer than surgery alone. Treatment takes 6 to 9 weeks and is conducted by our team member oncologist.
For more information on stomach cancer, visit this Cancer Research UK information page: http://cancerhelp.cancerresearchuk.org/type/stomach-cancer

Abdomen post laparoscopic resection of stomach cancer
GENERAL SURGERY
GROIN AND ABDOMINAL HERNIA REPAIRS
Groin and abdominal hernia are repaired by laparoscopy. Not all are suitable. Keyhole or laparoscopy is particularly beneficial in pain reduction and easy return to normal activities.Other hernias treated include umbilical, spigelian, incisional, and hernias of diaphragm (Bochdalek, Morgagni).
For more information on groin hernia repair, visit this Medline Plus information page: https://medlineplus.gov/ency/article/007406.htm
SPLENECTOMY (SPLEEN SURGERY)
This is usually performed when blood products have consumed by the spleen and the haematologist requests removal. It is done for conditions such as ITP, haemolytic anaemia, lymphoma, leukaemia and less usual problems (such as hypersplenism).Giant spleen can also be assisted by laparoscopy reducing the size of a cut and improving recovery.
For more information on spleen removal, visit this Medline Plus information page: https://medlineplus.gov/ency/article/002944.htm
DUODENUM AND SMALL BOWEL
Duodenum and small bowel operations are performed by keyhole where possible. Operations on the duodenum may be required for removal of cancers such as adenocarcinoma or as part of a larger operation e.g. Whipple procedure (pancreaticoduodenectomy).
All surgical procedures carry some risk. The information provided here is for general educational purposes only. Please contact Professor Falk to discuss the options that are appropriate for your individual situation.
For all appointments and enquiries contact us on:
FAX : +612 8580 5085